Decoding the Discomfort: What Is Chronic Pain?

So, dealing with pain that just won't quit? We get it. It's exhausting.
So, whether it's a back that's constantly aching, a nagging pelvic pain, or something totally different, what matters most is knowing what's causing it all. That's the first step to feeling better.
The main thing of this article is about chronic pain. We'll even zoom in on common things people struggle with, like chronic lower back pain, to really help you get your head around it. We'll help you figure out what's hurting you and why. We'll even touch on how chronic pain ICD 10 codes come into play when talking to your doctor or insurance.
Plus, we'll explore different chronic pain treatment options, from conventional medicine to alternative therapies like kratom and Journax, to help you find something that actually works.
And hey, while we're focused on relief, don't forget to give your mind a break too – sometimes a little distraction with some games for the brain can make a surprisingly big difference.

Chronic Pain Definition
Essentially, it's pain that sticks around for longer than the typical healing time – we’re usually talking 3 months or more. It's not just a longer-lasting version of a regular ache; it’s often a different beast altogether. This type of pain can also result from serious trauma.
Acute vs. Chronic
Acute is like that sharp sting when you stub your toe – immediate, intense, and (usually) short-lived. Chronic pain is the kind that lingers, often without an obvious cause or cure. The problem is, sometimes, with chronic regional pain syndrome, there's no good answer as to how the pain even started. Acute pain is a signal, chronic pain can feel like a broken alarm system.
Symptoms
You already know there's pain, but the chronic pain symptoms can vary wildly. Besides the constant throbbing, burning, or stabbing sensations, people often experience fatigue, sleep disturbances, mood swings (anxiety, signs of depression), and difficulty concentrating. It's a whole-body deal.

Neck | Chronic neck pain is a real drag, right? We're talking persistent stiffness, a dull ache that radiates into your shoulders or head, and sometimes even tingling or numbness down your arm. Causes can be anything from whiplash from a car accident years ago to simply hunching over a computer all day. The chronic back pain ICD 10 codes come into play when insurance needs to know what you're dealing with - there are codes for different types of neck issues. |
Back | Chronic low back pain ICD 10 is so common it's practically an epidemic. The pain can range from a constant, nagging ache to sharp, shooting pains that make it hard to move. It can radiate down your leg (sciatica), or just feel like a tight band across your lower back. The ICD 10 code for chronic back pain will depend on whether it’s disc-related, muscular, nerve-related, or something else entirely. Causes are varied: herniated discs, arthritis, spinal stenosis, muscle strains, and sometimes just plain wear and tear. Many people also have a hard time just sitting. |
Stomach | Chronic stomach pain is a beast. It's not just occasional indigestion. This is persistent cramping, bloating, nausea, and just an overall feeling of discomfort in your gut. It's often linked to underlying digestive issues like Irritable Bowel Syndrome (IBS), Crohn's disease, or even chronic gastritis. It can be super disruptive to daily life. |
Shoulder | You can get chronic shoulder pain from things like rotator cuff injuries, frozen shoulders, arthritis or even lack of sleep. It can make it hard to lift your arm, reach for things, or even sleep comfortably. |
Knee | Just like chronic shoulder pain, there is chronic knee pain. Osteoarthritis is a big culprit here, wearing down the cartilage in the joint. But it can also be from old sports injuries, bursitis, or patellar tendonitis. It can make walking, climbing stairs, or even just standing painful. |
Testicles | Men suffer with chronic testicular pain too, and it’s definitely something no one likes to talk about. The pain can be constant or intermittent, a dull ache or a sharp, stabbing sensation. Causes can include varicoceles, epididymitis, nerve damage, or sometimes, no identifiable cause at all. It can be a real quality-of-life killer. |
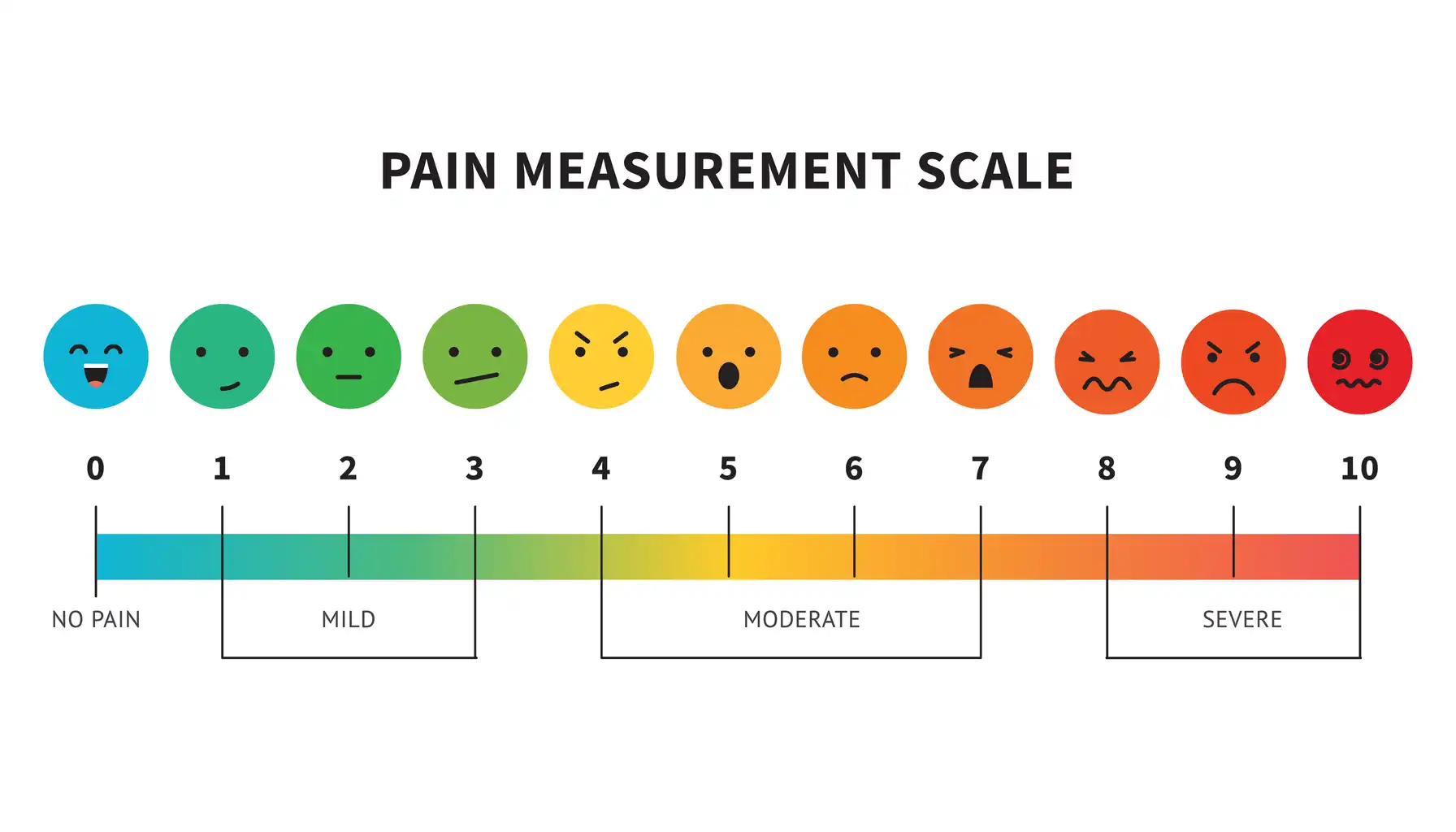
Chronic Pain Scale
What is ICD-10? Basically, it's the International Classification of Diseases, 10th Revision. Think of it as a massive, standardized list of codes used by healthcare providers and insurance companies to classify and track illnesses and conditions. It ensures everyone is speaking the same language when it comes to diagnoses.
Codes for Persistent Discomfort States
This is the big one – ICD 10 chronic pain syndrome. While it gives you something to put in your insurance, it can be pretty generic. If you are told by your doctor you have this syndrome then you might want to ask for something more specific.
While G89.4 is a general code, there are many other more specific ICD-10 codes that might apply, depending on where the trouble is.
For example, ICD 10 chronic back pain is a set of codes that more specifically describes the exact location.
So, if you have persistent discomfort after an injury or surgery, there's a code for that.
The chronic pain syndrome ICD 10 is a useful code for helping identify if you suffer from that condition.
There are even more precise codes for discomfort in the chest, pelvic region, or hip, depending on the underlying cause.
Knowing the ICD 10 code for chronic pain that relates to your specific areas will make everything easier.
What Is the Best Pain Medication for Chronic Pain
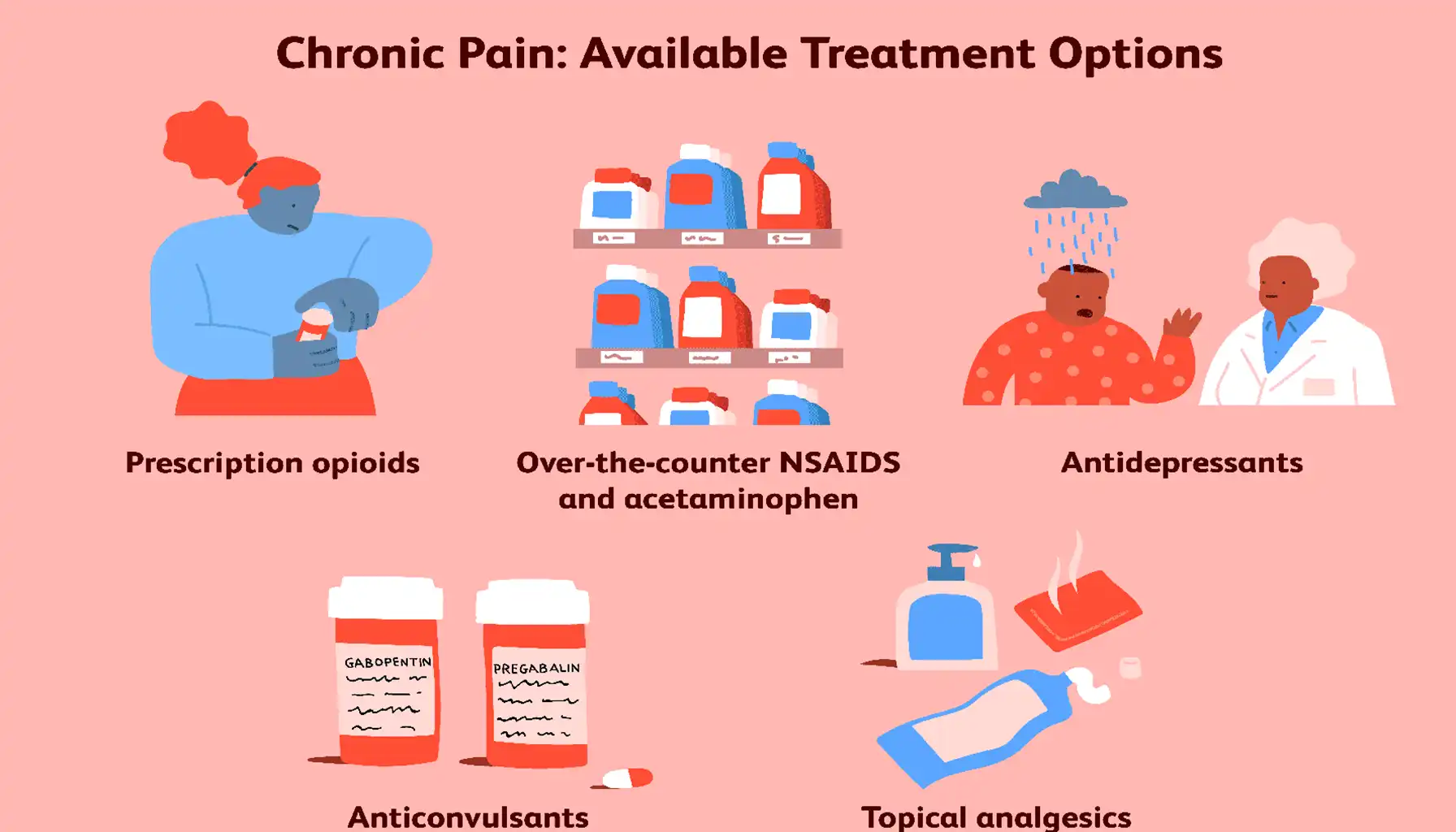
Over the Counter | Acetaminophen (Tylenol) | Works primarily on the central nervous system to reduce discomfort. It's generally safe but doesn't reduce inflammation. |
NSAIDs (Ibuprofen, Naproxen, Aspirin) | Reduce both discomfort *and* inflammation. However, long term use can increase the risk of stomach ulcers, kidney problems, and cardiovascular issues. | |
Prescription Medications | Opioids (Codeine, Oxycodone, Morphine) | Powerful analgesics that work on the central nervous system. They can be very effective for severe discomfort but carry a high risk of addiction, tolerance, and side effects like constipation, nausea, and drowsiness. |
Muscle Relaxants (Cyclobenzaprine, Diazepam) | Help relieve muscle spasms and tension, which can contribute to discomfort. However, they can also cause drowsiness and dizziness. | |
Antidepressants (Amitriptyline, Duloxetine) | Some antidepressants have been shown to reduce discomfort levels, even in people who aren't depressed. They work by affecting neurotransmitters in the brain that regulate mood and discomfort perception. | |
Anticonvulsants (Gabapentin, Pregabalin) | Originally developed for seizures, these medications can also help with nerve related discomfort, such as sciatica or diabetic neuropathy. |
The "Best" Analgesic
It isn't a universal solution. It depends on:
Type of Discomfort
Nerve discomfort often responds better to anticonvulsants or antidepressants, while muscle discomfort might respond better to muscle relaxants.
These medications impact the nervous system, particularly when we think about conditions like ADHD, classified as a chronic neurodevelopmental disorder – it highlights the complex ways our brains and bodies process signals, and how seemingly unrelated conditions might share underlying neurological pathways that can be addressed through targeted treatments.
Severity of Discomfort
Mild discomfort might be manageable with OTC medications, while severe discomfort might require prescription options.
Individual Factors
Age, other medical conditions, and potential drug interactions all play a role in choosing the right medication.
This process may involve trialing various medications, optimizing dosages, and vigilant monitoring for adverse effects
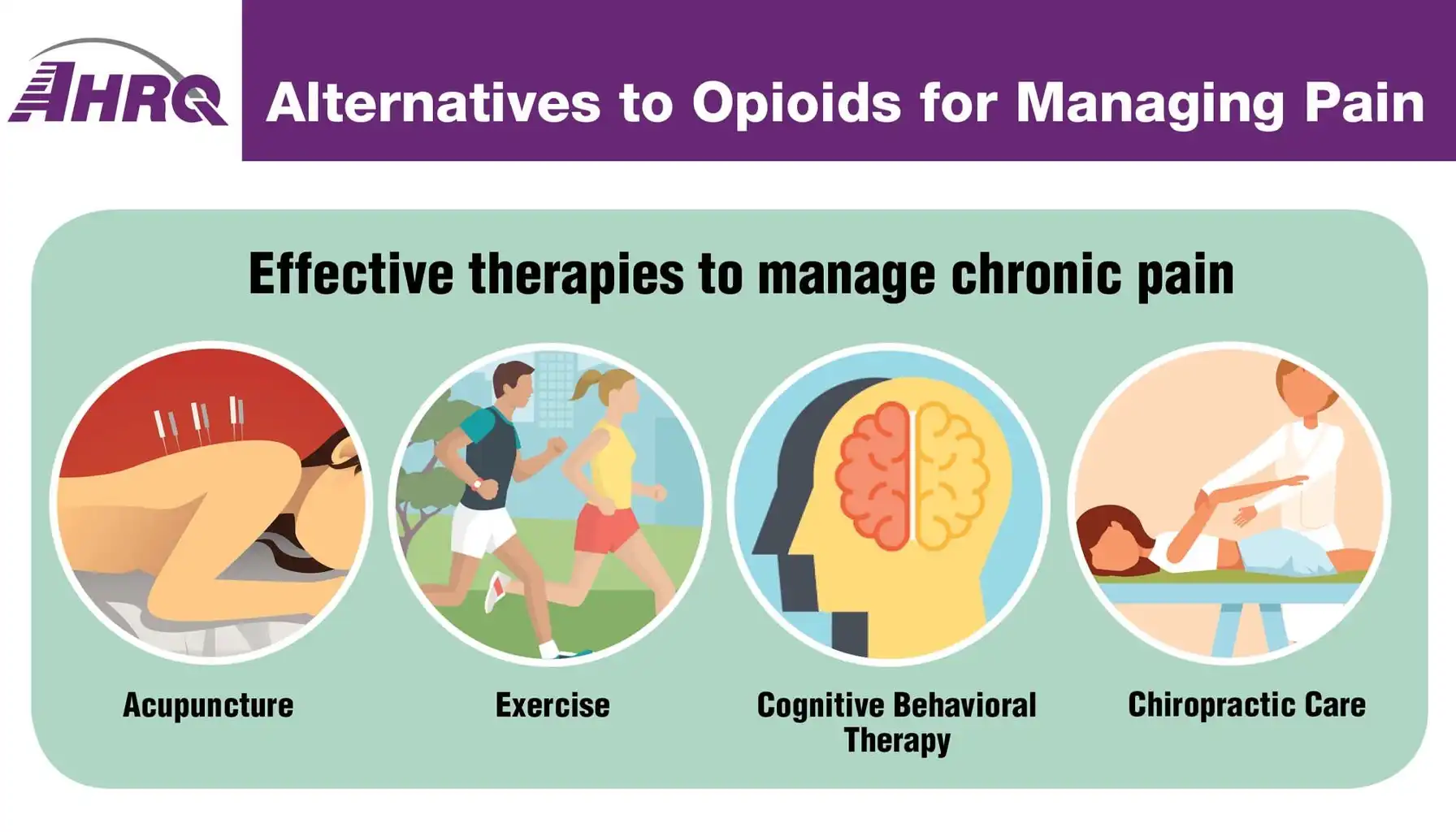
Alternative Methods
Kratom | Kratom is a tropical tree native to Southeast Asia. Within kratom's leaves lies a complex chemistry that yields a unique combination of effects – invigorating stimulation and soothing opioid-like sensations |
While some users claim that kratom helps alleviate discomfort, anxiety, depression, and opioid withdrawal symptoms, scientific evidence supporting these uses is limited | |
You might experience side effects: nausea, constipation, dizziness, drowsiness, or even liver problems. It can also be habit-forming, and if you stop using it suddenly, you may have withdrawal symptoms. Mixing Kratom with other drugs or alcohol can be dangerous. The Kratom for chronic pain approach should be taken with seriousness. | |
If you're considering kratom, talk to your doctor first. Start with a low dose, and monitor for side effects. Avoid using kratom daily for extended periods. | |
Journavx | Again, since "Journavx" is a hypothetical treatment. It's difficult to provide specific details. |
Look for peer-reviewed studies and reliable sources of information about the treatment. | |
Always talk to your doctor before trying any new treatment, especially if you have other medical conditions or are taking other medications. They can help you assess the potential benefits and risks. The Journavx for chronic pain route needs to be heavily researched before considering it. | |
Start with a low dose and monitor for any adverse reactions. |
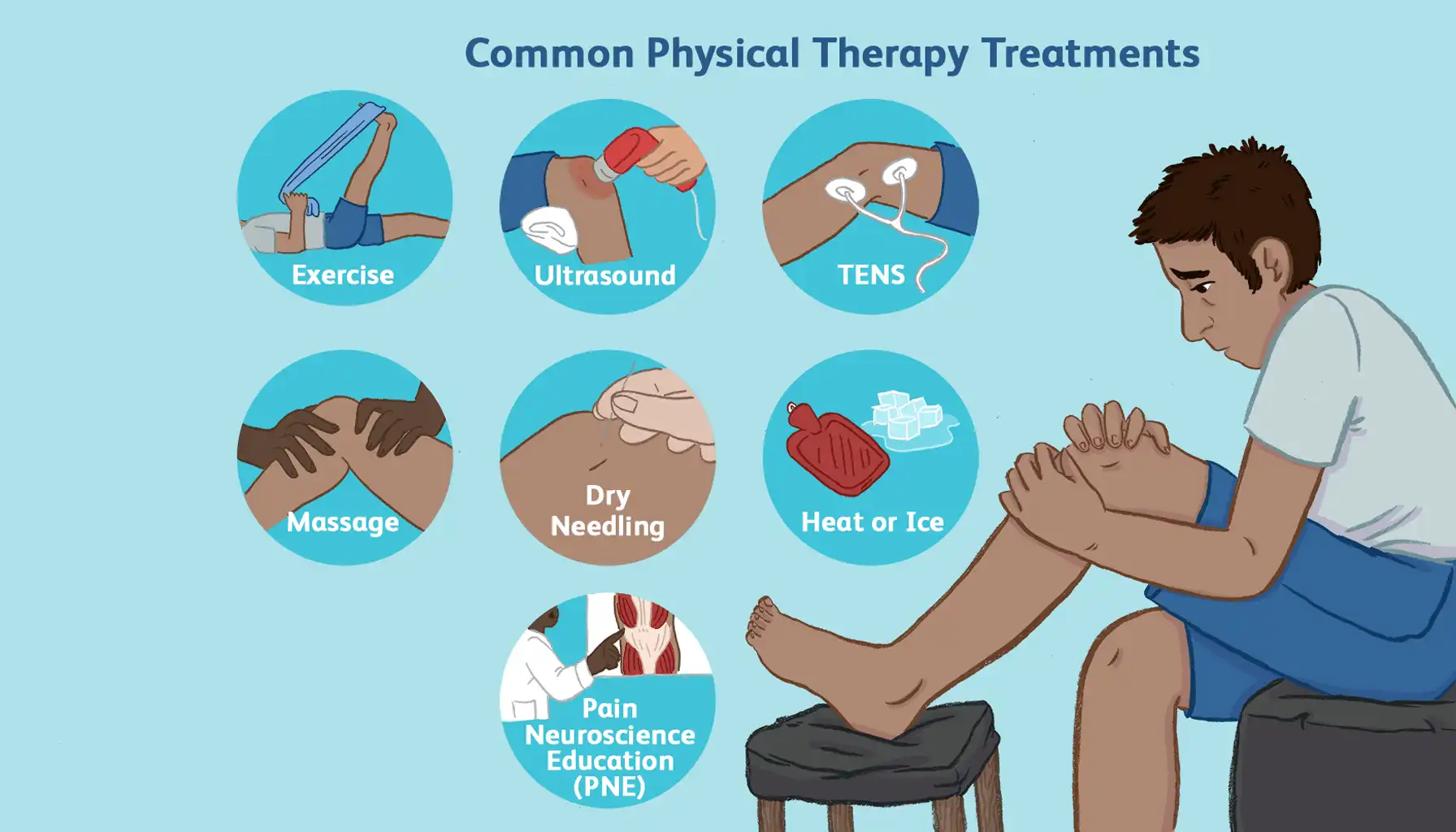
Physical Therapy and Rehabilitation
A physical therapist will conduct a thorough evaluation to identify the underlying causes of your discomfort, assess your range of motion, strength, posture, and movement patterns.
Based on the assessment, the physical therapist will develop a customized treatment plan that may include:
Strengthening exercises to support weak muscles, stretching exercises to improve flexibility, and range-of-motion exercises to restore joint mobility.
Hands-on techniques such as massage, joint mobilization, and soft tissue release to reduce muscle tension, improve circulation, and alleviate discomfort.
The physical therapist will educate you about your condition, proper body mechanics, and strategies for managing discomfort at home. Chronic back pain treatment often involves physical therapy.
The physical therapist will help you develop a long-term strategy for managing your discomfort and preventing future problems. Chronic pain management is all about working with people like physical therapists.





